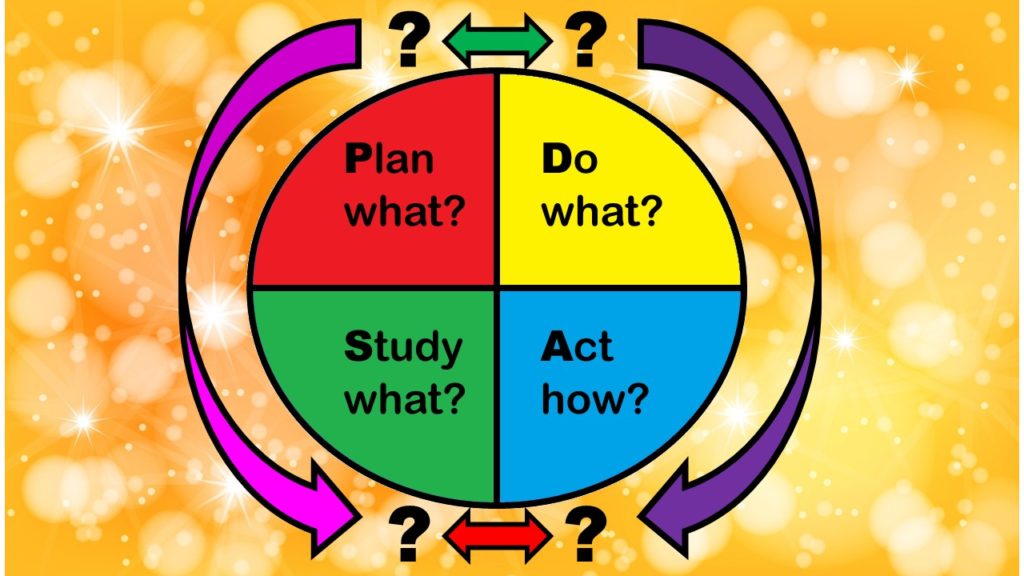
There are four stages of the PDSA model, which is the Plan-Do-Study-Act model that comes widely recommended as a framework to use to guide quality assurance and quality improvement (QA/QI) in healthcare. This series of blog posts summarizes the PDSA stages, presents actual use cases I have seen, and provides my assessment of its utility (along with recommendations for alternatives).
Stages of the PDSA Model Explained – Sort of
As I described in my introductory post to this series, there is the simple confusion introduced by the name Plan-Do-Study-Act, in that “do” can refer to “plan”, “study”, and “act”, and it’s not clear really what the difference is between “do” and “act”, and so on. I observed that the state where I grew up, Minnesota, has an explainer of the stages of the PDSA model on their health department’s website that was pretty good, which is what I’ll follow to try to explain each of these stages.
- Plan: In the Plan stage, you make a lot of documents – that’s clear, because there are a lot of steps under Plan – steps A through E. It is also very time-, cost- and effort-intensive. You need a team, and they need to do a lot of meetings to come up with the documentation to fulfill steps A through E.
- Do: The Do stage is really short. You apparently implement an “action plan” you made in the Plan stage. Again, in the Do stage, you are encouraged to make a lot of documentation that I’ve seen in management, but we don’t make in epidemiology: check sheets, flowcharts, swim lane maps, and run charts.
- Study: It is clear that you “study” something in the Study stage – but it actually says that you planned a study in the Plan stage, and data were gathered during Do stage. So this makes me ask – was the Plan stage there to create a research protocol, and the Do stage there to collect the data? Then the Study stage is for analyzing the data?
- Act: In the Act stage, you reflect on the outcomes of the Study stage. The way I read it, during the Act stage, then you set up another Plan stage, and the cycle keeps repeating itself.
The PDSA Model does not Capture all the Functions of QA/QI in Healthcare
I will explain what becomes very confusing about this model very quickly in QA/QI (in addition to the fact that the names of the stages do not provide a hint as to what happens in them). People in QA/QI do not think in “stages”. Stages imply linearity of time, where the effort passes through a sequence of phases, like a child going through a moody stage, and reemerging her sunny usual self.
That’s not really how QA/QI departments function as a whole, or how employees function independently. They are not like researchers who are working on projects at different stages. They are actually people with titles like “Infectious Disease Director” who are responsible for a variety of QA/QI functions not reflected in the PDSA model.
I have needed to make my own model to guide my work with my QA/QI customers, so here’s what I did. Instead of stages, I defined functions of a QA/QI department. These functions can be best seen as going on all the time, with different people doing different things at different times, but overall, making sure the QA/QI department fulfills these functions.
Five Functions of a QA/QI Department in Healthcare
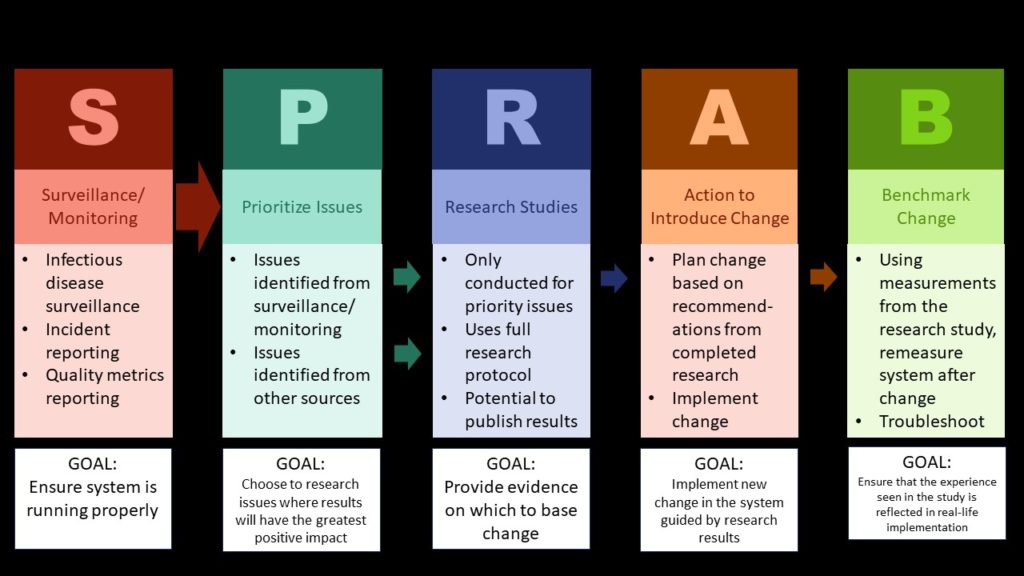
Here are the five functions of a QA/QI department in my view:
- Surveillance – This refers to regular, ongoing data collection into systems used for monitoring quality. An example includes tracking falls in a fall database, and analyzing it monthly to see if there are emerging trends.
- Prioritize – QA/QI leaders cannot fix everything. They need an approach to prioritizing which issues to work on so as to get the greatest gain in quality, cost-savings, or some other goal. For example, if surveillance shows that falls are an emerging issue that rises to a high level of priority, leaders should then prioritize this issue.
- Research – In order to fix anything in healthcare, you need real-world evidence from your own healthcare facility. So if you see an uptick in falls and want to figure out if an intervention will work, you have to do little research studies with the settings where your surveillance says the extra falls are taking place. That’s the only way to figure out what interventions work in your setting, and which ones you might want to roll out across the system.
Imagine you do a research study, and find out the falls were caused by people tripping on things that don’t really need to be on the floor. Your intervention to implement to prevent falls would involve educating staff about maintaining floor cleanliness. So let’s say you did another research study and found an effective educational intervention, so you decide to implement it systemwide. - Action to introduce change – Or – alternatively – let’s say you do absolutely no research, but your health agency comes and insists you put railings up in places you didn’t have them before. Both “training” and “handrails” are actions to introduce change. It might improve things, and it might not. But actually implementing that action is a step itself. Whether you are training people or putting up railings, it’s going to take a while.
- Benchmark change – For all situations where you did an action to introduce change, you will need to benchmark the change. In the example with falls, this will be easy – you already have a falls database, and you can just rerun the numbers. But in other cases, benchmarking the impact of the change might not be as easy. It still needs to be done in order to see if the action worked, and if not, what our next steps are.
How do the Stages of the PDSA Relate to the Functions of a QA/QI Department?
This was my next question: What does the PDSA have to do with these different QA/QI functions, which all seem pretty independent of each other? I figured there might be a connection somehow between each stage and a variety of the functions, but I really wasn’t sure of the connection, and there is literally no documentation online where the PDSA acknowledges that all these functions somehow occur in QA/QI.
I actually had to see some real customers who had tried to apply the PDSA, and I queried them as to their experience in order to try to puzzle this out. I finally now kind of understand what the PDSA model’s authors might have been getting at.
In my next post in the series, where I explain the evidence (or lack thereof) behind the PDSA, I provide some insight into what I believe the PDSA architects might have been thinking about when developing the model. While on the surface, their thinking does not look incorrect, in practice, the PDSA model tends to break down. I was able to identify where I think the error was in their philosophy, which I explain in my next post.
Updated June 17, 2021. Added blog menu July 19, 2021. Added new banners March 6, 2023. Updated banners June 28, 2024.
Read all the posts in the series!
What are the stages of the PDSA model, and how do they relate to the functions of a QA/QI department in healthcare? The answers are not straightforward. I examine these issues in this blog post.